- India Sees 9% Drop in Foreign Tourists as Bangladesh Visits Plunge |
- Dhaka Urges Restraint in Pakistan-Afghan War |
- Guterres Urges Action on Safe Migration Pact |
- OpenAI Raises $110B in Amazon-Led Funding |
- Puppet show enchants Children as Boi Mela comes alive on day 2 |
HIV/AIDS Funding Cuts Threaten Decades of Global Progress
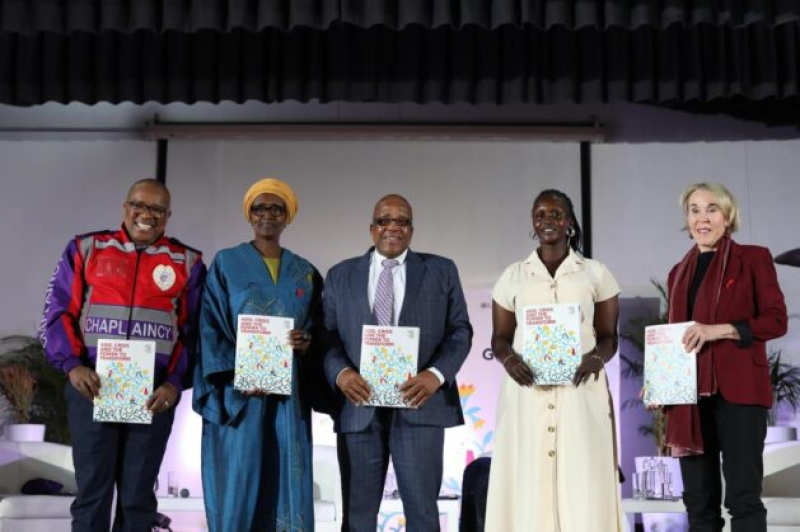
UNAIDS report launch highlighted that 9.2 million people lacked HIV treatment in 2024. Pictured: Rev. Mbulelo Dyasi, Winnie Byanyima, Aaron Motsoaledi, Juwan Betty Wani, and Helen Rees.
UNAIDS has described the current funding crisis as a ticking time bomb, warning that cuts to the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) could result in four million unnecessary AIDS-related deaths by 2029.
A historic withdrawal of global HIV/AIDS funding threatens to derail decades of hard-won progress in the fight against AIDS, according to UNAIDS’ annual report titled AIDS, Crisis and the Power to Transform. The funding shortfall—driven by sudden, massive cuts from international donors—is already dismantling frontline services, disrupting lifesaving treatments for millions, and endangering countless lives in the world’s most vulnerable communities.
“This is not just a funding gap—it’s a ticking time bomb,” said UNAIDS Executive Director Winnie Byanyima.
Despite major progress in 2024, including a 40% reduction in new HIV infections and a 56% decrease in AIDS-related deaths since 2010, the restriction of international aid—which funds 80% of prevention efforts in low- and middle-income countries—could prove disastrous. The report, based largely on data from late 2024, stated that ending AIDS as a public health threat by 2030 remained within reach.
However, in early 2025, the United States announced a shift in its foreign assistance strategy, leading to the withdrawal of support from organisations like PEPFAR, which had pledged $4.3 billion in 2025. PEPFAR is a critical provider of HIV testing and treatment services in the hardest-hit countries. Such a drastic move could trigger ripple effects, potentially prompting other major donors to follow suit. The report projected that if global funding continues to shrink, an additional six million HIV infections and four million AIDS-related deaths could occur by 2029.
At a press briefing, Assistant Secretary-General for UNAIDS Angeli Achrekar highlighted PEPFAR's role since its launch in 2003, calling it one of the most successful public health initiatives. She expressed hope that other nations and organisations would step in to uphold the global promise to end AIDS without losing the progress made.
Achrekar noted “acute shifts” in commitment from countries less directly affected by HIV/AIDS following the U.S. funding cut.
UNAIDS also reported a worrying rise in laws criminalising populations most at risk of HIV, which increases stigma and contributes to gender-based violence and non-consensual sex—two major drivers of HIV transmission. The report noted that the groups most often excluded from care were children with HIV and young women, largely due to government crackdowns on HIV-related human rights efforts.
These punitive laws include criminalising HIV exposure under general criminal laws, as well as prosecuting sex work, same-sex sexual activity, transgender identity, and the possession of small quantities of drugs. The combination of such laws and reduced funding poses a deadly threat to HIV-positive individuals.
Meanwhile, scientific breakthroughs have brought promise—such as long-acting medications to prevent HIV infection. Health workers have seen success with annual injections, monthly tablets, and tried-and-tested methods like condom distribution and access to clean needles for drug users. But global conflicts have disrupted supply chains, affecting access to critical products like PrEP in countries that depend on them.
While many of the most affected countries have pledged more domestic funding and strengthened community efforts, the loss of international healthcare personnel and disrupted supply chains cannot be easily resolved. Restructuring healthcare systems takes time—something people living with HIV cannot afford to lose.
Sub-Saharan Africa, which in 2024 was home to half of the 9.2 million people lacking HIV treatment, has been particularly impacted. Most child infections still occur in the region, where economic challenges—such as debt, sluggish growth, and weak tax systems—limit governments' ability to fund domestic HIV responses.
Despite the funding setback, some progress has been sustained. South Africa now finances 77% of its AIDS response, and its 2025 budget includes a 3.3% annual increase in HIV and tuberculosis funding for the next three years. As of December 2024, seven countries in sub-Saharan Africa had reached the UNAIDS 95-95-95 goals: 95% of people living with HIV knowing their status, 95% of those receiving treatment, and 95% achieving viral suppression. UNAIDS stressed the need to expand this success globally.
Achrekar emphasised that prevention remains under-prioritised: “We will never be able to turn off the tap of new infections without focusing on prevention as well.”
She reiterated the need for the most affected countries to build self-reliant, resilient healthcare systems for sustainable HIV prevention and treatment.
Praising the Global South for taking ownership of treatment efforts, she urged the international community to renew its solidarity.
“The HIV response was forged in crisis and built to be resilient. We need, and are calling for, global solidarity once again to rebuild a nationally owned, sustainable and inclusive multi-sectoral HIV response,” she said.